Benign prostatic hyperplasia (BPH) is a common health trouble in mature men. It’s characterised by the progressive enlargement of the prostate gland by the non-malignant proliferation of smooth muscle and epithelial cells. This enlargement manifests clinically as lower urinary tract symptoms (LUTS) such as urgency, frequency, urinary retention, straining to urinate, a weak urinary stream or nocturia.1
The histologic prevalence of BPH has been assessed around the world and is approximately 10% for men in their 30s, 20% for men in their 40s, climbs to 50–60% for men in their 60s and peaks at 80–90% for men in their 70s and 80s.2
The diagnosis and treatment of BPH has been calculated to be the largest segment of urologic practice, representing 23% of total visits and 12.2 million men being managed each year in the US.3
BPH and its related manifestations may significantly alter the quality of life of mature men suffering from this condition. Although a variety of different medical treatments are currently available for BPH, alternative natural solutions also exist, such as saw palmetto, nettle roots, Pygeum africanum, pumpkin seed oil, etc. Some hexanic extracts of saw palmetto even show efficacies that are equivalent to medicinal products … but without the side-effects.4
An innovative saw palmetto extract: Vi-spo
Vidya Herbs has developed a solvent-free beta-sitosterol-enriched (3%) saw palmetto extract. It is obtained from non-GMO Serenoa repens berries that are cultivated without pesticides using a 100% green CO2-SC extraction process and chromatographic purification.
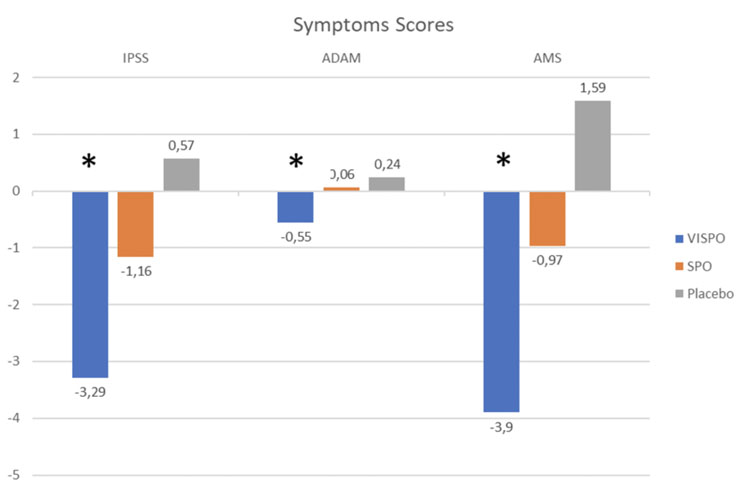
Figure 1: symptom scores (*: p<0.05)
Laboratory experiments have shown that Vi-spo exerts its beneficial activity through three complementary mechanisms of action. It inhibits 5-α-reductase activity to limit the transformation of testosterone to dihydrotestosterone. It modulates the apoptosis of prostate cells, promoting the regular renewal that can slow down prostate growth.
It also modulates inflammation and reduces the risk factors associated with cancer development.5 Owing to its specific mechanisms of action, Vi-spo could also be a suitable natural solution for androgenic alopecia.6,7
The efficacy of Vi-spo has been compared with a conventional saw palmetto extract and a placebo in a double-blind, randomised, placebo-controlled clinical trial. This trial was done with 99 male subjects (40–65 years old) for 84 days. Subjects consumed either 200 mg of Vi-spo (VISPO), 200 mg of traditional saw palmetto extract (SPO) or the placebo (200 mg), twice a day after food.
Effects were evaluated with instrumental measurements and officially recognised questionnaires. Symptom assessment was performed using the International Prostate Symptom Score (IPSS), the Aging Male Symptom (AMS) scale and the Androgen Deficiency in the Aging Male (ADAM) questionnaire.
Quality of life was rated with the SF-12 survey. Considering the evolution of BPH, uroflowmetry and post-void residual urine volume (PVR) were measured. At the end of the trial, Vi-spo showed no clinical or blood chemistry changes and was very well tolerated; no adverse effects were reported and none of the subjects reported any severe adverse events.
At the end of the study, a significant reduction from the baseline IPSS score (–3.29 ± 3.21 p<0.05) was observed in the VISPO group. A non-significant (-1.16 ± 3.38 p>0.05) reduction was noticed in the SPO group and an increase (+0.57 ± 5.22 p>0.05) was recorded in the placebo group.
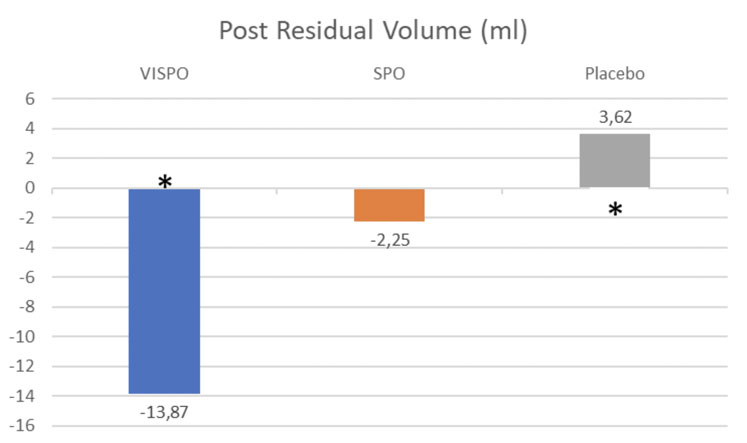
Figure 2: Post residual volume (* = p<0.05)
The ADAM questionnaire confirmed these results and demonstrated a significant reduction (–0.55 ± 1.09 p<0.05) for the VISPO group. A corresponding increase was noted in the SPO (+0.06 ± 0.93 p>0.05) and placebo (+0.24 ± 0.99 p>0.05) groups.
The AMS scale also confirmed the results, showing a significant reduction (–3.90 ± 4.74 p<0.05) from baseline in the VISPO group, a non-significant reduction (–0.97 ± 4.33 p>0.05) in the SPO group and a significant increase (+1.59 ± 2.34 p>0.05) in the placebo group (Figure 1).
Interestingly, the perceived improvements recorded in the questionnaires were confirmed by the instrumental physiological assessments, the Post Residual Urine Volume (PRV) and the uroflowmetry.
A significant reduction from the PRV baseline was only observed in the VISPO group (–13.87 ± 13.90 p<0.05), whereas a non-significant reduction was seen in the SPO group (–2.25 ± 11.16 p>0.05). A significant increase in PVR was observed in the placebo group (+3.62 ± 8.80 p>0.05), as shown in Figure 2.
This voiding capacity improvement of the bladder was confirmed by the uroflowmetric assessment of both maximum and average urine flow rates. A significant improvement in the former was observed in the VISPO group (+2.39 ± 1.57 p>0.05), whereas a significant-yet-smaller improvement was recorded in the SPO group (+0.58 ± 13.90 p<0.05).
The placebo group demonstrated a non-significant reduction of the maximum flow rate (–0.55 ± 2.35 p>0.05).
Average urine flow rate was improved in the same way. A significant improvement was observed in the VISPO group (+1.06 ± 1.55 p<0.05), a non-significant improvement was seen in the SPO group (+0.23 ± 1.59 p<0.05) and significant reduction was measured in the placebo group (–0.86 ± 1.27 p<0.05). See Figure 3.
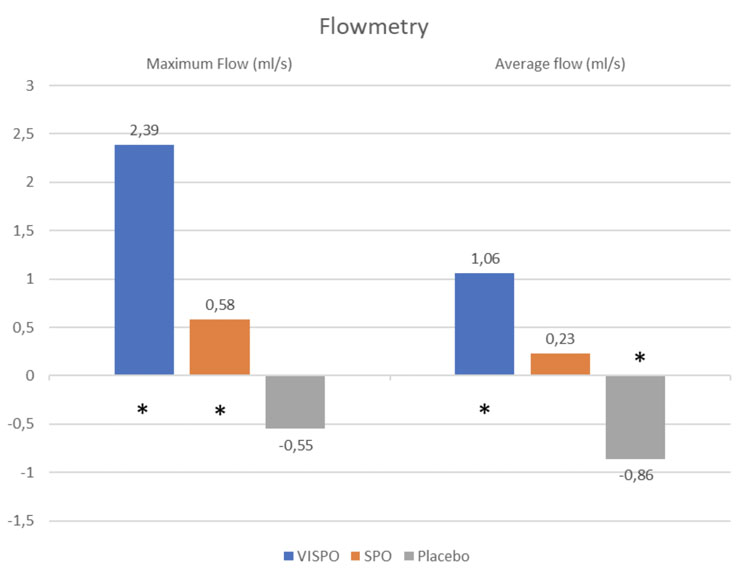
Figure 3: flowmetry (* = p<0.05)
Considering the results from the questionnaires and the physiological assessments, it makes sense that the global quality of life of the VISPO group participants improved. The SF-12 questionnaire noted a significant improvement in the VISPO group (+1.81 ± 1.97 p<0.05), whereas a smaller non-significant improvement was recorded in the SPO group (+0.45 ± 1.73 p>0.05).
A significant decrease in quality of life was observed in the placebo group (–0.76 ± 1.79 p<0.05). See Figure 4.
The results show that Vi-spo is more efficacious than a conventional saw palmetto extract compared with a placebo. Vi-spo subjects were the only ones that improved their physiological functions (according to PRV and uroflowmetry assessments), their symptoms, urinary issues and quality of life.
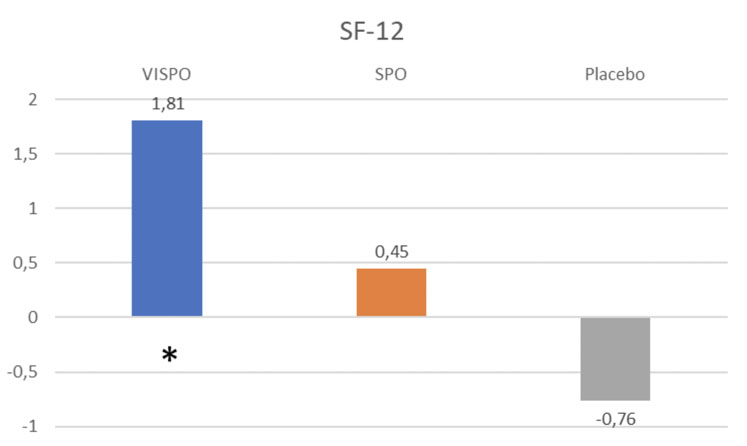
Figure 4: quality of life score SF-12 (* = p<0.05)
For the conventional saw palmetto group, the results generally trended well but showed no significant developments. Logically, the physiological status, indication and quality of life all degraded during the study in the placebo group.
An holistic ingredient for men with BPH
By improving the urinary comfort of mature men and by enhancing their physiological functions, it is clear that Vi-spo augmented their quality of life in a variety of important areas (as reported in the questionnaires).
Sexual life: It has been demonstrated that urinary issues correlate with sexual discomfort.8 In the AMS subscale analysis dealing with a lack of sexual pleasure and a reduced desire for sexual intercourse, a significant improvement was noted in the VISPO group with a mean score reduction of –1.35 ± 1.82 (p<0.05) compared with the SPO (0.00 ± 1.37 p>0.05) and the placebo (+0.79 ± 1.32 p<0.05) groups.
Well-being and vitality: The benefits of Vi-spo in terms of energy, well-being, pain and tiredness were also demonstrated by the SF-12 physical subscale (PCS-12). It showed a significant improvement in the VISPO group (+0.97 ± 1.02 p<0.05), whereas the SPO group showed a non-significant improvement (+0.29 ± 0.97 p>0.05) and the placebo group worsened (–0.41 ± 1.05 p<0.05).
Mood: The benefits of Vi-spo on mood, irritability, anxiety and nervousness were also established by the AMS psychological subscale and demonstrated a significant score reduction in the VISPO group (–2.39 ± 2.72 p<0.05). In contrast, the SPO group showed a non-significant score reduction (–0.74 ± 2.37 p>0.05) and the placebo group showed a significant increase (+0.52 ± 0.83 p<0.05).
Conclusion
The results of the clinical trial demonstrated that Vi-spo is more efficacious than a conventional saw palmetto extract to treat BPH. But, more than that, it’s also a powerful ingredient that has a key role to play in the healthy lives of mature men.
Indeed, with positive effects on the symptoms of BPH and by restoring physiological urinary functions, it also improves the sexual life, mood and well-being of mature men. By restoring their urinary comfort and virility, Vi-spo both restores a sense of self-confidence and contributes to healthy ageing.
References
- E.M. Bortnick, V. Simma-Chiang and S.A. Kaplan, “Long-Term Consequences of Medical Therapy for Benign Prostatic Hyperplasia,” Rev. Urol. 21(4), 154–157 (2019).
- C.G. Roehrborn, “Benign Prostatic Hyperplasia: An Overview,” Rev. Urol. 7 (Suppl. 9), S3–S14 (2005).
- C. Vuichoud and K.R. Loughlin, “Benign Prostatic Hyperplasia: Epidemiology, Economics and Evaluation,” Can. J. Urol. 22(Suppl. 1), 1–6 (2015).
- A. Alcaraz, et al., “Quality of Life in Patients with Lower Urinary Tract Symptoms Associated with BPH: Change Over Time in Real-Life Practice According to Treatment: The QUALIPROST Study,” Int. Urol. Nephrol. 48(5), 645–656 (2016).
- H.V. Sudeep, et al., “A Phytosterol-Enriched Saw Palmetto Supercritical CO2 Extract Ameliorates Testosterone-Induced Benign Prostatic Hyperplasia by Regulating the Inflammatory and Apoptotic Proteins in a Rat Model,” BMC Complement. Altern. Med. 19(1), 270 (2019): doi: 10.1186/s12906-019-2697-z.
- M.B. Morgan and P. Rose, “An Investigation of Apoptosis in Androgenetic Alopecia,” Ann. Clin. Lab. Sci. 33(1), 107–112 (2003).
- M. El-Domyati, et al., “Evaluation of Apoptosis Regulatory Markers in Androgenetic Alopecia,” J. Cosmet. Dermatol. 9(4), 267–275 (2010).
- J.C. Nickel, M. Elhilali and G. Vallancien, “Benign Prostatic Hyperplasia (BPH) and Prostatitis: Prevalence of Painful Ejaculation in Men with Clinical BPH,” BJU International 95, 571–574 (2005).
