There’s no greater joy than finding out that there’s a baby on the way. When a woman who wants to become a mother first discovers she is pregnant, she thinks about what she needs to do to ensure her baby arrives healthy and ready to grow. Quatrefolic® folate protects both mother and baby throughout pregnancy, especially women with a genetic mutation of which they might not be aware.
Did you know that a significant percentage of Asian women have a gene that prohibits theirbodies from fully absorbing folic acid? This is known as MTHFR polymorphism (or mutation).1–4 MTHFR is responsible for converting folic acid into folate; so, if a woman with this
mutation supplements with folic acid, they are probably not obtaining its benefit. However, supplementing directly with folate bypasses this conversion, enabling women with MTHFR polymorphism to get enough of this B vitamin as recommended.
Vitamin B9 has long been known as the pregnancy vitamin and is typically found in the marketplace as folic acid. However, a better form of vitamin B9 is more biologically useful and, therefore, valuable. Folate is a water-soluble vitamin that’s essential for rapid cell growth and division, maintaining new cells and making DNA and RNA during foetal development.
Pregnant women have a 5–10-fold higher requirement than their non-pregnant counterparts
Adequate folate intake is particularly important for pregnant women, with a 5–10-fold higher requirement than their non-pregnant counterparts. Owing to a commonly occurring genetic mutation, folic acid cannot be used optimally by everyone; this makes folate the superior choice for supplements, beverages and foods that target women for prenatal and natal health.
Recent research distinguishes between naturally occurring folates and folic acid; these terms are often used interchangeably but — although similar — they’re not the same.5 The natural form of folate (5-methyltetrahydrofolate [5-MTHF]) is clinically proven to be a more effective alternative to folic acid for pregnant women. This is because, for many, taking folic acid may not provide the crucial protective benefits for the mother and developing foetus.
The Homocysteine factor
Homocysteine (Hcy), a common amino acid that circulates in the bloodstream, has a biochemical relationship with folate. However, excessive Hcy is an independent causal factor of pregnancy complications and adverse neonatal outcomes. Thus, the goal for women who are or are seeking to become pregnant is to ensure that their Hcy levels are in healthy ranges.
This is especially true for women who have MTHFR polymorphism, a known antagonist of folate-dependent Hcy metabolism. According to research, the normal range of Hcy during pregnancy is 3.9–7.3 mmol/L before 16 gestational weeks, 3.5–5.3 mmol/L between 20 and 24 gestational weeks and 3.3–7.5 mmol/L after 36 weeks.6
Women with high Hcy levels are often administered tests to see if the MTHFR mutation is the most common type: 677CT heterozygous and 677TT homozygous. In Asia, 43.8% of MTHFR polymorphism is heterozygous and 14% is homozygous (Figure 1).7 This test is important because research demonstrates that women with homozygous MTHFR polymorphism have significantly lower folate levels than heterozygous; they also exhibit much higher Hcy concentrations, which is more pronounced in women with low folate intake.8
Pregnant women or those actively trying to become pregnant prioritise reducing and maintaining low Hcy levels
It is critical that pregnant women or those actively trying to become pregnant prioritise reducing and maintaining low Hcy levels, as numerous studies have found that high Hcy levels are associated with several pregnancy complications. These include recurrent pregnancy loss, neural tube defects, pre-eclampsia, preterm delivery, placental abruption, foetal growth restriction and gestational diabetes mellitus.6,9–15 Evidence also shows that high Hcy levels are associated with neonatal birth weight (the higher the maternal levels, the lower the weight).16
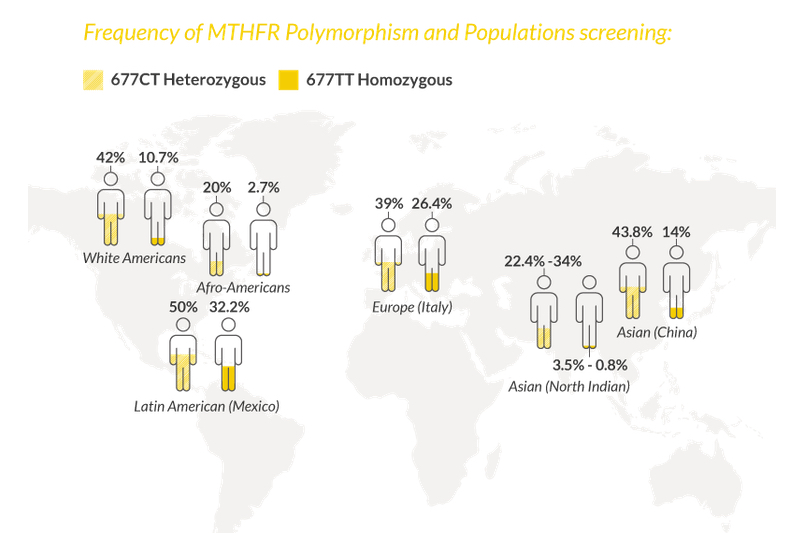
In Asia, 43.8% of MTHFR polymorphism is heterozygous and 14% is homozygous.
How reducing Hcy with folate lowers pregnancy-associated risks
The good news for all mothers-to-be — including those with the MTHFR polymorphism — is that folate supports healthy Hcy levels. Two months of daily folate consumption combined with B6 and B12 was more effective at reducing Hcy blood levels than folic acid.17
Several studies show that supplementation with folate can have measurably protective results. Pregnant women who supplemented with Quatrefolic folate until the 24th week of pregnancy showed higher levels of the active folate in their blood than the same dose of folic acid. This study also confirmed the importance of folate supplementation in terms of avoiding the development of neural tube defects.18
In one study looking at women experiencing difficulties conceiving, Quatrefolic folate in combination with vitamins B12 and B6 (Normocis Inpha Duemila) was compared with folic acid in 269 women undergoing assisted reproductive technology. A higher percentage of women in the vitamin B complex group had a clinical pregnancy and live birth compared with the women consuming folic acid. The authors concluded that women who supplemented with Quatrefolic and vitamin B12 have a higher chance of clinical pregnancy and live birth.19 The clinically validated alternative to folic acid for healthy pregnancy and foetal development: supplementation with 400 μg of Quatrefolic (plus B6 and B12) for 2 months was more effective at reducing Hcy blood levels than folic acid.17
After the baby arrives
Post-partum depression is a serious condition that impairs the bonding between the new mother and her infant; it also presents other symptoms that reduce quality of life and mental wellness. In Asian nations, post-partum depression affects approximately 3.5–63.3% of women (Malaysians had the lowest and Pakistanis had the highest).20 
Post-partum risk may be mediated with folate supplementation. Results of a cohort study showed that the prevalence of post-partum depression was significantly higher among pregnant women taking folic acid for 6 months or less than those who reported consuming folic acid for more than 6 months during pregnancy. It is logical to conclude that these results would be more profound if folate were used instead of folic acid.21
When formulating multivitamins and other supplements for women in their childbearing years and who become pregnant, consider
using 5-methylfolate as Quatrefolic instead of folic acid to ensure this critical B vitamin is utilised by all your potential female consumers.
References
1 A.M. Henderson, et al., J. Nutr. 148, 855–890 (2018).
2 Y. Lamers, et al., Am. J. Clin. Nutr. 84, 156–161 (2006).
3 B.J. Venn, et al., Am. J. Clin. Nutr. 77, 658–662 (2003).
4 Y. Lamers, et al., Am. J. Clin. Nutr. 79, 473–478 (2004).
5 C.M. Ulrich and J.D. Potter, Cancer Epidemiol. Biomarkers Prev. 15(2), 189–193 (2006).
6 C. Dai, et al., Biomed. Res. Int. 2021, 6652231 (2021).
7 B. Wilcken, et al., J. Med. Genet. 40(8), 619–625 (2003).
8 A. De Bree, et al., Am. J. Clin. Nut. 77(3), 687–693 (2003).
9 X Zhao, et al., Medicine 99(40), e21962 (2020).
10 U. Yadav, et al., Birth Defects Res. 113(7), 589–600 (2021).
11 N.C. Serrano, et al., PLOS One 13(12), e0208137 (2018).
12 X. Qiu, J. Matern. Fetal Neonatal Med. 31(20), 2673–2677 (2018).
13 T.A. Goddijn-Wessel, et al., Eur. J. Obstet. Gynecol. Reprod. Biol. 66(1), 23–29 (1996).
14 H.L. Jiang, et al., Genet. Mol. Res. 15(4), 4 (2016): doi:10.4238/gmr15048890.
15 M.A. Guven, et al., Arch. Gynecol. Obstet. 274(6), 333–337 (2006).
16 S. Cawley, et al., J. Matern. Fetal Neonatal. Med. 33(18), 3045–3049 (2020).
17 A. Mazza, et al., JBRHA 30(3), 921–927 (2016).
18 D. Dell'Edera, et al., Eur. Rev. Med. Pharmacol. Sci. 21(14), 3305–3311 (2017).
19 M. Cirillo, Int. J. Environ. Res. Public Health 18(23), 12280 (2021).
20 P. Klainin and D.G. Arthur, Int. J. Nurs. Stud. 46(10), 1355–1373 (2009).
21 J. Yan, et al., Nutrients 9(11), 1206 (2017).

