Although vitamin D3 is capable of initiating several important biological processes, vitamin K2 is essential for their completion and expression. In this article, Lena Leder from Kappa Bioscience will present the latest scientific research about the important role these two vitamins play in a number of key health areas and will highlight opportunities for innovation for nutraceutical manufacturers.
What, how and why: the facts about vitamin K2
The K family of vitamins form an integral part of the nutritional tapestry that’s needed to keep bodily functions running as normal. All categorised as fat-soluble vitamins, there are in total 12 forms of the vitamin K molecule. Each type of vitamin K2 delivers a subtly different effect on the body; but, for the purposes of this article, we’ll focus on the two forms that are most abundant in the human diet.
K2 MK-4: This form of the molecule represents a smaller proportion of total vitamin K2 intake but is relatively easily to obtain through the consumption of animal products. MK-4’s main use is supporting bone and heart health.
K2 MK-7: The most bioactive of the vitamin K family is also the least naturally available. K2 MK-7 is only found in specific fermented foods, such as natto cheese. Consequently, the diets of most Western consumers are severely lacking in this nutrient. This is particularly concerning considering that the molecule plays an important role in regulating calcium metabolism.
Consumers and nutraceutical brands alike are becoming more familiar with the applications and importance of vitamin K. At the same time, however, most remain unaware of the benefits that vitamin K2 MK-7 can offer both alone and in combination with a molecule already famous for its health-supporting properties: vitamin D3.
Introducing the perfect pair
Vitamin D is a small molecule that’s capable of entering any cell and reaching its nucleus (where vital genetic information is stored).1 It interacts with the promotor regions of human cells, which “decide” whether a gene should be switched on or off, resulting in increased production of the specific protein that the gene is responsible for encoding.2
Several types of cells contain control regions that interact with both vitamin D3 and K2. Two of the best-known examples of these vitamin K-dependent proteins (VKDPs) are osteocalcin (OC) and matrix Gla protein (MGP). Vitamin D3 molecules are capable of promoting the expression of these calcium-binding proteins; alone, however, it can only express them in their inactive or uncarboxylated form.3
This leaves the body unable to effectively regulate the integration of calcium from the intestines, potentially leading to diminished bone mass, higher fracture risk and the calcification of arteries and other soft tissues.
An adequate intake of vitamin K2 ensures the effective carboxylation of OC and MGP proteins, which in turn helps the body to bind calcium to bones — while keeping levels in the bloodstream at the correct quantities to avoid vascular calcification.
With such a variety of potential benefits, scientists have begun referring to the interaction between vitamins K2 and D3 as a true “synergy.” The two molecules combine to produce more valuable effects than they are capable of alone. With this in mind, let’s explore the specific health areas in which this perfect pair offers the most pronounced benefits for improved health and well-being.
Bone health
The bone matrix contains cells called osteoblasts and osteoclasts that are responsible for breaking down and building up bone in an ongoing remodelling process. Osteoblasts secrete a protein called osteocalcin into the blood which, when activated by vitamin K2, binds to calcium and transports it from the blood and into the bones.
Osteoblasts then integrate this calcium into the bone matrix, increasing the bone’s mineral density and strength. As part of the remodelling cycle, osteoclasts remove old or damaged bone so that it can be replaced with new cells.
As we age, this process of regeneration naturally slows, making bones lighter, more porous and therefore more susceptible to fractures. High levels of uncarboxylated osteocalcin as a result of inadequate vitamin K2 and D3 intake at any stage of life produce similar effects to the natural ageing process.4
In a landmark 1997 study, researchers set out to compare the effect of vitamin K on osteocalcin both with and without the presence of vitamin D3. After introducing lab-grown osteoblasts to vitamins D3 and K2 in isolation and combination, the scientists measured the volume of osteocalcin that the cells were able to produce.
The results were fairly conclusive. The osteoblasts exposed to higher doses of vitamin D3 alone exhibited higher production and accumulation levels of osteocalcin in the extracellular matrix. In the cultures that were treated with a combination of vitamins, however, vitamin K2 was shown to enhance the D3-mediated osteocalcin production and accumulation (Figure 1).

Figure 1: The effect of vitamin K on osteocalcin in the presence or absence of vitamin D3
The study effectively demonstrates that vitamin K2, induced by a dose of 1,25(OH)2D3 in cultured human osteoblasts, enhances both the accumulation of osteocalcin and its production. The implications of this research are supported by a recently conducted meta-analysis that aimed to evaluate the effects of vitamin D3 and K2 synergy on human health — particularly bone mineral density (BMD).
Here too, the researchers concluded that the combination of vitamins D3 and K2 can significantly increase total BMD and decrease undercarboxylated osteocalcin, and that the effects are more favourable when the two are used in combination.5
The conclusions we can draw from this body of evidence are clear. The perfect pair combine to increase bone strength and density, suggesting that supplementation with vitamins D3 and K2 could help to reduce the risk of fractures and bone loss in older individuals while also supporting the development of strong bones in children.
Heart health
Cardiovascular health is another key area of study for scientists investigating the benefits of this perfect pair. Vitamins D3 and K2 have been shown to improve heart health by reducing the amount of “free” calcium in the bloodstream. A diverse range of studies exist to support this conclusion, including an investigation into the interplay between D3 and K2 in arterial calcification rates of rats (Figure 2).
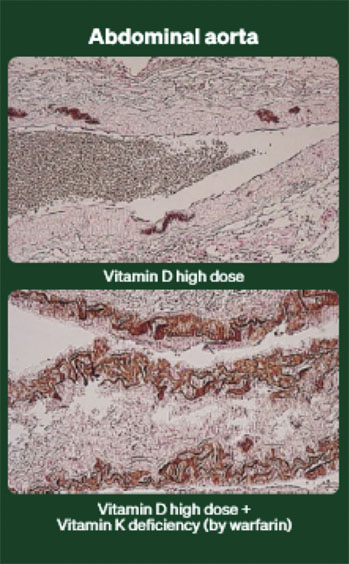
Figure 2: Arterial calcification: vitamins K and D interplay in rats6
As shown in these images, subjects exposed to high doses of vitamin D, without the addition of sufficient vitamin K, exhibited far higher levels of arterial calcification, leading to a dramatically increased mortality rate.6
These results suggest the presence of vitamin D alone is not enough to prevent harmful levels of arterial calcification, a hypothesis supported by the results of a human study into the effect of vitamins D3 and K2 on the expression and activation of MGP.
As discussed above, vitamin D is capable of “turning on” the expression of MGP within the gene; but, without K2, the protein remains in its inactive or uncarboxylated state. In their 2008 study, Fu et al. found that when exposed to sufficient amounts of K2, MGP can be carboxylated and effectively bind calcium in the vascular system — decreasing the risk of vascular mineralisation.7
The benefits of D3/K2 for heart health and general longevity have been made evident in a number of other studies, which have shown that the adequate intake of D3 and K2 can help to reduce mortality risk, maintain healthy blood pressure levels and reduce arterial stiffness.8–10 Clearly these tiny molecules can have a big impact on keeping hearts healthy.
Immunity
Finally, in recent years, scientists have begun investigating the potentially beneficial effects that D3 and K2 can have on the human immune system. There is a growing body of evidence to suggest that increased levels of vitamin D can reduce the risk of COVID-19 infection … but could the addition of K2 help improve health outcomes even further?11
In a study published in March this year, a group of researchers set out to investigate the effect that vitamin D and K status had on 135 hospitalised COVID-19 patients in relation to inflammatory response, elastic fibre degradation and clinical outcomes.12
They did this by measuring circulating 25-hydroxyvitamin D (25[OH]D) and desphospho-uncarboxylated Matrix Gla-Protein (dp-ucMGP) to determine vitamin status, and comparing this against the severity of inflammatory response in patients as defined by the level of interleukin (IL)-6 in their blood.
The study found significant differences between the disease outcomes of patients with high and low levels of IL-6, suggesting it is a central component of the destructive inflammatory processes in COVID-19.12
It also found a clear association between Dp-ucMGP (the protein used to determine vitamin K status) and IL-6 levels, potentially pointing to a correlation between vitamin K deficiency and the severity of COVID-19 infection.
Further studies are needed to confirm whether vitamin K supplementation, combined with vitamin D or not, can actually improve clinical outcomes associated with COVID-19, but research such as this points to the exciting possibility that the perfect pair could deliver a whole new set of immunity-based benefits.
A new world of opportunities — with the right K2
What then can nutraceutical manufactures take away from the emerging science surrounding vitamin D3 and K2? In short, this perfect pair present a golden opportunity for brands to appeal to health-conscious consumers who are keen to maximise their overall well-being.
As the body of scientific evidence grows to support the beneficial effects of vitamin K2, so too is awareness about the purity and quality of the different brands of K2 available on the market.
At Kappa Bioscience, we help manufacturers to unlock the benefits of D3/K2 with our pure, 99.7% all-trans vitamin K2 MK-7 supplement, K2VITAL, and K2VITAL DELTA, an innovative double-encapsulated exceptionally stable vitamin K2. These versatile, easy to use solutions are fully bioactive, ensuring that consumers can experience the full benefits for their bones, hearts and bodies.
References
- https://lpi.oregonstate.edu/mic/vitamins/vitamin-D.
- www.frontiersin.org/article/10.3389/fphys.2019.00194.
- Y. Koshihara and K. Hoshi, “Vitamin K2 Enhances Osteocalcin Accumulation in the Extracellular Matrix of Human Osteoblasts In Vitro,” J. Bone Miner. Res. 12(3), 431–438 (1997).
- M.J. Shearer, “The Roles of Vitamins D and K in Bone Health and Osteoporosis Prevention,” Proc. Nutr. Soc. 56(3), 915–937 (1997).
- X. Kuang, et al., “The Combination Effect of Vitamin K and Vitamin D on Human Bone Quality: A Meta-Analysis of Randomized Controlled Trials,” Food Funct. 11(4), 3280–3297 (2020).
- P.A. Price, et al., “Warfarin-Induced Artery Calcification is Accelerated by Growth and Vitamin D,” Arteriosclerosis, Thrombosis and Vascular Biology 20, 317–327 (2000).
- X. Fu, et al., “9-Cis Retinoic Acid Reduces 1alpha,25-Dihydroxycholecalciferol-Induced Renal Calcification by Altering Vitamin K-Dependent Gamma-Carboxylation of Matrix Gamma-Carboxyglutamic Acid Protein in A/J Male Mice,” J. Nutr. 138(12), 2337–2341 (2008).
- A.J. van Ballegooijen, et al., “Combined Low Vitamin D and K Status Amplifies Mortality Risk: A Prospective Study,” European Journal of Nutrition 60, 1645–1654 (2021).
- A.J. van Ballegooijen, et al., “Joint Association of Low Vitamin D and Vitamin K Status with Blood Pressure and Hypertension,” Hypertension 69(6), 1165–1172 (2017).
- O. Mayer Jr, et al., “Synergistic Effect of Low K and D Vitamin Status on Arterial Stiffness in a General Population,” J. Nutr. Biochem. 46, 83–89 (2017).
- A. Teshome, et al., “The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis,” Front. Public Health 9, 624559 (2021).
- www.frontiersin.org/article/10.3389/fnut.2021.761191.
