Despite COVID-19 being a respiratory disease, its complications are also cardiovascular. Early clinical data indicate both the susceptibility and outcomes of COVID-19 to be strongly associated with cardiovascular disease (CVD).1–7
A high prevalence of pre-existing CVD has been observed in COVID-19 patients, with the comorbidities being associated with increased mortality.8–11
Conversely, COVID-19 seems to promote the development of cardiovascular disorders, such as myocardial injury, arrhythmias, acute coronary syndrome (ACS) and venous thromboembolism.12–14
Concerns about the cardiovascular outcomes of SARS-CoV-2 infection started during the early stages of the pandemic. A research paper from China found that 20% of COVID-19 hospitalised patients developed heart disease and that thromboembolic events happened in 31% of those in the intensive care unit.12,15
Another article from Germany reported ongoing myocardial inflammation in 60% of 100 recently recovered patients with COVID-19.16
Vitamin D supplementation and immune support
Overcoming micronutrient deficiencies could become part of an effective strategy in the fight against COVID-19. The evidence for vitamin D supplementation is already compelling … and fast gaining government and public attention.
Although supplementation with vitamins D and K2 cannot be considered preventive or curative against COVID-19, growing scientific evidence shows a correlation between low serum D/K2 levels and more severe outcomes for the disease.
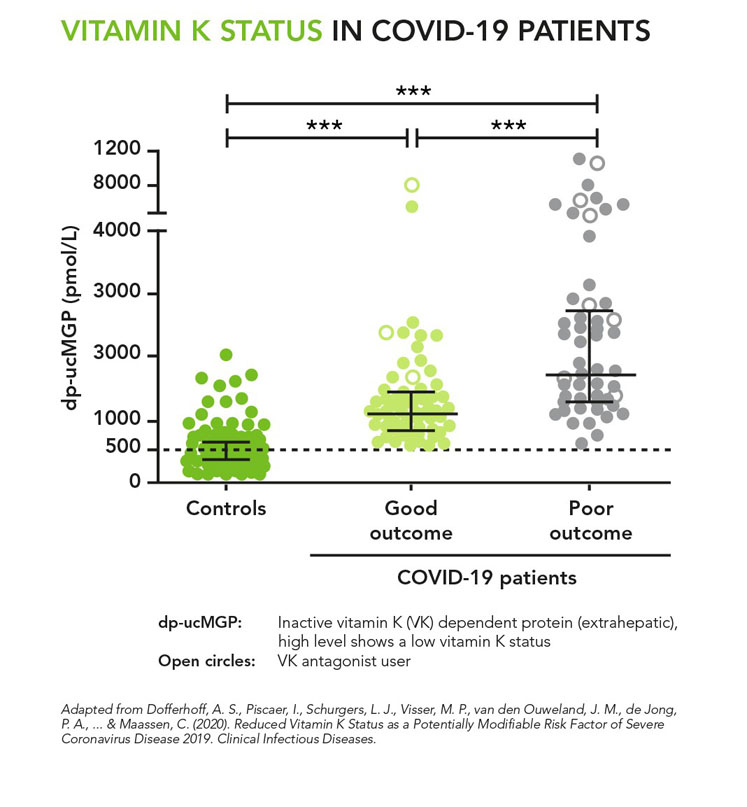
Figure 1: Vitamin K status in COVID-19 patients
Vitamin D is known for its multiple health implications, including cardiovascular and immune system effects. As such, vitamin D supplementation to support the immune response to COVID-19 is increasingly being investigated.
Several meta-analyses have already demonstrated vitamin D benefits against respiratory tract infections: low levels of vitamin D were associated with a higher risk for infection and symptoms severity.17–20
Similar findings have been published regarding the association between low vitamin D levels and a higher risk of SARS-CoV-2 infection.21–30
Questions remain regarding an effective dose. Because vitamin D is so important for the normal functioning of our metabolism, daily requirements may be much higher in times of infection. Suggested doses of vitamin D to support the immune system are usually above the recommendation levels (600 IU) proposed by EFSA and the US FDA, which scientists say were not set with immune outcomes in mind.
Some studies cite a daily dose of 4000-5000 IU for virus-free people to maintain a healthy vitamin D status. Others state that this should be doubled to 10,000 IU daily for a few weeks to rapidly raise vitamin D levels.31
Since May 2020, the French Academy of Medicine now recommends vitamin D supplementation levels of 800–1000 IU/day in people younger than 60 as soon as a COVID-19 diagnosis is confirmed. For those older than 60 with a vitamin D deficiency, a loading dose of 50,000–100,000 IU could “help to limit respiratory complications.”
Notably, vitamin D administration is recommended to avoid the so-called cytokine storm — a violent inflammatory response of the immune system that is often harmful and can be fatal.
If vitamin D intake is generally regarded as safe, high doses of vitamin D can induce short-term hypercalcaemia, a transient increase in serum calcium levels.32 Calcium, although vital for normal functioning of the human body, has deleterious effects if not properly regulated. The deposition of calcium in the blood vessels or on elastic fibres in the lungs can lead to damage.33–36
Vitamin K2
This is where vitamin K2 comes into play. The calcium-binding proteins involved in preventing soft-tissue calcification are K2-dependent; as such, they remain inactive in the absence of sufficient K2 intake.37–40
In bones, they incorporate calcium into the bone matrix. In soft tissues such as blood vessels or the lungs, they prevent calcium deposition, elastic fibre degradation, thrombosis and inflammation.
Recent studies evaluating serum K2 levels in COVID-19 hospitalised patients found that patients with poor outcomes of COVID-19 had the lowest levels of vitamin K2.41 In comparison, people tested negative for SARS-CoV-2 infection showed adequate vitamin K2 levels (see Figure 1).
“Although more research is needed, we found data in our study that suggests that vitamin K deficiency may be the missing link between lung damage and thrombosis in COVID-19. Considering that vitamin K is important for regulating lung health and blood clotting, vitamin K deficiency during COVID-19 may make both those problems worse,” says Dr Rob Janssen, Researcher at Canisius Wilhelmina Hospital, Nijmegen, Netherlands.
Consequently, he and his team published a paper to explain the potential mechanisms behind the action of vitamin K2.32 Janssen suggests that vitamin K2 deficiency is the link between thrombosis and lung damage, two of the most serious outcomes of COVID-19 (Figure 2).
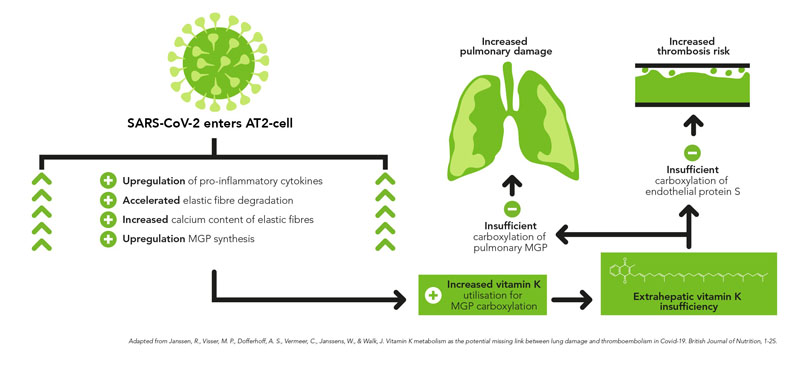
Figure 2: Proposed sequential steps linking SARS-CoV-2 pneumonia to vitamin K insufficiency, pulmonary damage and thrombogenicity
The review, published in the British Journal of Nutrition also highlights the critical link between vitamin D3 and vitamin K2. Hypercalcaemia induced by vitamin D administration, which has become part of certain clinical treatment protocols for COVID-19, could lead to accelerated calcification and the degradation of elastic fibres.
“The administration of vitamin D in a state of vitamin K2 deficiency may thus endanger the health of both respiratory and cardiovascular systems,” notes Dr Janssen.
In SARS-CoV-2-infected patients, low vitamin K2 status may impact COVID-19 pathogenesis even further. Some K2-dependent proteins play a key role in protecting our cardiovascular health. In the absence of sufficient amounts of vitamin K2, matrix Gla protein (MGP) is not able to prevent calcification.
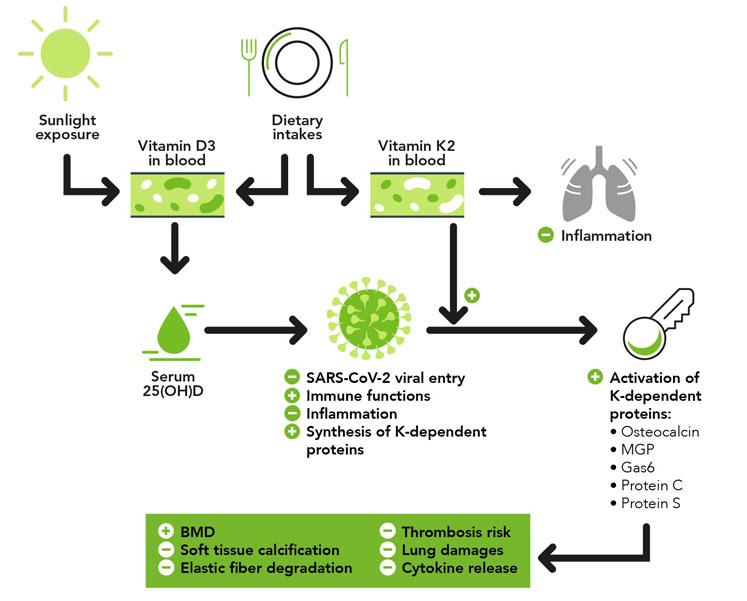
Figure 3: The combined immune health benefits of vitamins D and K2
That may result in elastic fibre degradation, damage occurring in the lungs and stiffening of the blood vessels. Vascular calcification limits the body’s ability to circulate oxygen-rich blood and is an important risk factor for cardiovascular disease.
Similarly, protein S, which plays a key role in thrombosis prevention, requires K2 for its activation. Low K2 levels may therefore aggravate the coagulopathy and thrombosis formation observed in COVID-19 patients (Figure 3).
Like vitamin D, vitamin K2 has been shown to act as an anti-inflammatory agent by downregulating several metabolic pathways involved in inflammation and cytokine release.42–44
Kappa Bioscience is currently investing in research — through collaborations with universities and hospitals — to better understand the implications of vitamin K2 deficiency in COVID-19 pathogenesis and severity.
Conclusion
High vitamin D supplementation, as increasingly investigated and recommended by medical doctors and health authorities, can come with a downside. Considering the scientific evidence, it seems prudent to recommend combining its supplementation with vitamin K2.
For a complete list of the references cited in this article, please contact the author at info@kappabio.com.
