Market trend analysts report that sports supplements are not only being consumed by trained athletes; a growing number of active people consume them as part of a healthy lifestyle. The prevention of health issues and the strengthening of natural defences is a growing trend in this category. Indeed, it has been shown that exercise can induce perturbations in the body’s natural defences, increasing the risk of upper respiratory tract disorders and gastrointestinal discomfort.
For example, in 2012, out of the 10,568 athletes competing at the London Summer Olympics, 7.2% reported an illness, 46% of which were infections.1 The gut microbiota plays a central role in the body’s homeostasis. In 2006, a clinical study using probiotics in sport nutrition was published that showed a potential supporting effect in training athletes. This was confirmed with time and another randomised double-blind placebo-controlled trial was published in March 2016 that showed that the probiotic Lactobacillus helveticus LAFTI L10 was able to significantly reduce the duration of upper respiratory tract infection episodes — as well as the number of symptoms per episode — in training athletes, which has been further correlated to the significant increase of immune markers.2 Such studies confirm that probiotic benefits go well beyond gut health and indicate that they represent potential solutions for the booming sports or active nutrition market.
Restoring an athlete’s natural defences
Both cellular and humoral immune responses (secretion of IgA and antimicrobial protein, granulocyte activity) can undergo acute and chronic changes during intense exercise. The relationship between intense physical exercise and immunity has been described as a J-shaped curve (Figure 1). It appears that people are more prone to bacterial and viral infections following intense training. This phenomenon can last for up to 72 hours.3
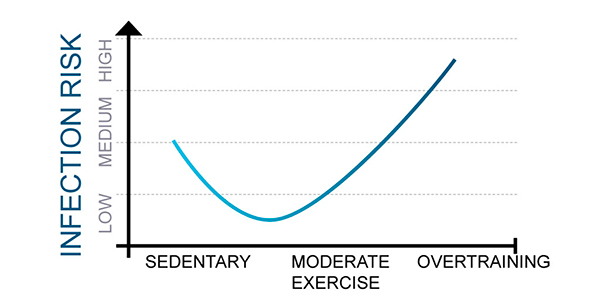
Figure 1: The relationship between intense exercise and infection risk3
As the gut harbours more than 60% of the body’s immune cells, probiotics have become increasingly well recognised for their immune response benefits. Both mechanistic and clinical evidence indicate their potential to modulate and restore a normal immune response. This could certainly apply to sports nutrition when the immune response is suboptimal. A specific probiotic strain, Lactobacillus helveticus LAFTI L10 is particularly well-documented in athletes. Preclinical and clinical studies show that this probiotic strain has the ability to boost an immune response lowered by exercise in athletes.4
Clancy published the first trial conducted in athletes with probiotics in 2006.5 This pre-post intervention study was conducted on two groups of well-trained recreational athletes: 18 “healthy” ones and nine others suffering from over-training, recurrent sore throats and impaired performance. Before the probiotic treatment, the two groups showed a significant difference in interferon-g (IFN-g) levels — a cytokine known to protect against virus infections — which confirmed the consequence of intense training on immunity.
L. helveticus LAFTI L10 supplementation succeeded in restoring the immune response: after one month of probiotic administration, the levels of IFN-γ gsecreted by CD4+ T cells in fatigued athletes was restored (Figure 2). For the healthy group, salivary IFN-g levels also increased. The results of the study were correlated with previous in vivo studies in which L. helveticus LAFTI L10 induced the production of IFN-g in challenged animals (data not shown).
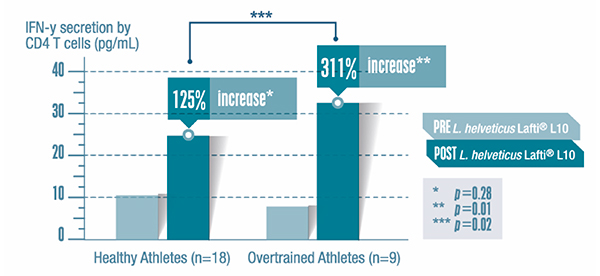
Figure 2: Effect of 4-week L. helveticus LAFTI L10 treatment on the levels of mediator cells implicated in the immune response (INF-g) in athletes5
Reducing the risk of infection
Impaired immunity, combined with the hyperventilation that naturally occurs during exercise, contributes to a higher susceptibility to upper respiratory tract disorders (URT) in sportspeople. Hyperventilation induces mechanical damage to the respiratory tract, resulting in inflammation, asthma-like symptoms, a runny nose, fatigue and ultimately, fever, representing 30–40% of reported URT disorders in athletes.6,7
URT infections (URTIs) are a common cause of missed training or a lost competition and can affect performance. Hence, prevention is key, especially in the winter or when preparing for an important event. In 2016, a new clinical study was conducted on elite athletes during winter to evaluate the clinical and immunomodulatory effects of L. helveticus LAFTI L10, confirming previous findings.2 The 39 elite athletes enrolled in the study, 18–28 years old, were training for more than 11 hours per week in various sports; they received a probiotic treatment or a placebo for 14 weeks during the winter. This randomised, double-blind placebo controlled study looked at the severity, the incidence and the duration of URTIs episodes using validated scales and monitored biological immune markers. Secondary endpoints included a self-rated state of mood evaluation (POMS) to record any changes in behaviour and performances after the treatment.
The study showed that L. helveticus LAFTI L10 supplementation
- significantly shortened the average duration of URTIs by 3.4 days (7.25 days with the probiotic versus 10.64 with the placebo, p<0.05); see Figure 3
- significantly decreased the number of symptoms by approximately 29% (4.92 symptoms with the probiotic versus 6.91 with the placebo, p<0.05; URTI severity tended to decrease (p=0.078)
- increased the self-rated sense of vigour and tended to reduce the proportion of athletes reporting impaired training.
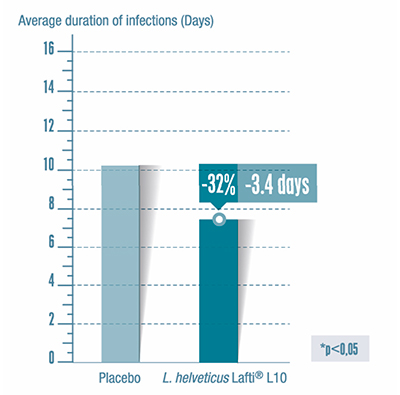
Figure 3: Effect of probiotic treatment on average infection duration (URTI)2
Moreover, several changes in immune markers were recorded during the study in the probiotic group; such parameters are not commonly measured in probiotic sport studies. It was shown, for example, that the CD4+/CD8+ ratio increased by 8% in the probiotic group.
Finally, an earlier study conducted with the same probiotic strain in stressed students corroborated its protective potential when the subjects’ natural defences were challenged. In this study, 300 students, who normally suffer from at least two colds a year, were enrolled during the winter and divided into two groups (placebo and probiotic). Results of the study showed a significant reduction of the number of systemic symptoms by 12.2% with L. helveticus LAFTI L10. Moreover, the symptoms were less severe in this group. As a result, the probiotic significantly reduced the need for medication: the total number of medicated days (mainly analgesics) was reduced by 23%.8
That gut feeling
Gastrointestinal (GI) functions are also affected during exercise. The body directs its blood supply to the lungs and heart, to the detriment of other organs. For example, the smooth muscles of the gut can be deprived of up to 80% of their normal blood flow. This phenomenon of hypoperfusion can lead to perturbations in gut motility and intestinal epithelial cell damage, increasing gut permeability.9 Exercise-induced GI disturbances manifest in diarrhoea, vomiting and acid reflux, which can impair training and performance.
The ability of probiotics to balance and restore the intestinal microbial ecosystem is well known. Their modes of action are increasingly well documented and it has been shown that probiotic bacteria can adhere to the gut epithelium, preventing the adhesion of pathogens. Certain strains have the ability to enhance the gut barrier function. For example, it has been shown that L. helveticus Rosell-52 reinforces the gut barrier by strengthening the junctions between epithelial cells, leading to a reduced incidence of infection.10 The probiotic yeast S. boulardii communicates with cells lining the gut (enterocytes) and helps to preserve their integrity and normal metabolism.11 In addition, this probiotic yeast also shows a positive effect on the junctions of epithelial cells.12
GI health and diarrhoea prevention are strong areas of clinical evidence for probiotics. For example, the association of Lactobacillus rhamnosus Rosell-11 and Lactobacillus helveticus Rosell-52 is the subject of 26 clinical studies in digestive health, showing benefits in the prevention of antibiotic-associated and acute diarrhoea, gastroenteritis and management of irritable bowel syndrome (IBS).13 Around 80 published clinical trials conducted with S. boulardii indicate its ability to prevent GI tract infections and manage IBS. Thus, probiotics appear to play a role in alleviating the impact of exercise on GI functions.
In conclusion, probiotics represent a novel approach to sports nutrition. Their ability to restore and maintain the microfloral balance and immunity can prevent respiratory tract infections and alleviate exercise-induced GI disturbances in active people, from professional athletes to everyday sportspeople. Moreover, probiotics have proven their ability to interact with the brain-gut axis and alleviate the psychological and physiological symptoms of stress and contribute to mood balance — a key issue for athletes and active people. As such, even if they can not make us run faster, probiotics can help to support a healthy body and mind, essential to sport performance.
References
- L. Engebretsen, et al., “Sport Injuries and Illnesses During the London Summer Olympic Games 2012,” Br. J. Sports Med. 47, 407–414 (2013).
- D. Marinkovic, et al., “Lactobacillus helveticus LAFTI L10 Supplementation Reduces Respiratory Infection Duration in a Cohort of Elite Athletes: A Randomized Double-Blind Placebo-Controlled Trial,” Applied Physiology, Nutrition, and Metabolism 41(7), 782–789 (2016).
- D.C. Nieman, “Immunonutrition Support for Athletes,” Nutrition Reviews 66(6), 310–320 (2008).
- G. Paturi, et al., “Immune Enhancing Effects of Lactobacillus acidophilus LAFTI L10 and Lactobacillus paracasei LAFTI L26 in Mice,” Int. J. Food Microbiol. 115(1), 115–118 (2007).
- R.L. Clancy, et al., “Reversal in Fatigued Athletes of a Defect in Interferon-gγ Secretion After Administration of Lactobacillus acidophilus,” Br. J. Sports Med. 40, 351–354 (2006).
- L. Spence, et al., “Incidence, Etiology and Symptomatology of Upper Respiratory Illness in Elite Athletes,” Med. Sci. Sports Exerc. 39(4), 577–586 (2007).
- S. Bermon, “Airway Inflammation and Respiratory Tract Infections in Athletes: Is There a Link?” Exerc. Immunol. Rev. 13, 6–14 (2007).
- R. Eccles, et al., “A Study on Winter Infections in Students,” Internal Report (Common Cold Centre and Healthcare Clinical Trials, Cardiff School of Biosciences, Cardiff University, 2008).
- K. van Wijck, et al., “Exercise-Induced Splanchnic Hypoperfusion Results in Gut Dysfunction in Healthy Men,” PLoS One 6(7): e22366 (2011).
- P.M. Sherman, et al., “Probiotics Reduce Enterohemorrhagic Escherichia coli O157:H7 and Enteropathogenic E. coli O127:H6-Induced Changes in Polarized T84 Epithelial Cell Monolayers by Reducing Bacterial Adhesion and Cytoskeletal Rearrangements,” Infection and Immunity 73(8), 5183–5188 (2005).
- T. Kelesidis and C. Pothoulakis, “Efficacy and Safety of the Probiotic Saccharomyces boulardii for the Prevention and Therapy of Gastrointestinal Disorders,” Ther. Adv. Gastroenterol. 5(2), 111–125 (2012).
- L.V. McFarland, “Systematic Review and Meta-Analysis of Saccharomyces boulardii in Adult Patients,” World Journal of Gastroenterology 16(18), 2202–2222 (2010).
- L.M. Foster, T.A. Tompkins and W.J. Dahl, “A Comprehensive Post-Market Review of Studies on a Probiotic Product Containing Lactobacillus helveticus R0052 and Lactobacillus rhamnosus R0011,” Beneficial Microbes 2(4), 319–334 (2011).





