Depending on the product type, the specifications for these conditions will vary. For example, to prevent microbial contamination during production, it is necessary for the product to be manufactured in a sterile cleanroom environment.
Use of cleanroom facilities ensures that the processing environment is rigidly regulated; these are highly controlled environments that are classified, depending on their intended use, by a number of international standards. Such standards include EU GMP Annex 1 (soon to be updated, more on this later) or USP chapter <1116> Microbiological Evaluation of Clean Rooms and Other Controlled Environments.
Sterility in cleanroom environments is maintained through the physical operation of heating ventilation and air conditioning (HVAC) to ensure a high throughput of fresh filtered air, as well as other contamination control measures. These other measures include stringent cleaning routines and the separation of personnel from product by gowning and the use of barrier technology such as isolators. To demonstrate the ongoing sterility of cleanroom environments and ensure that the environment is controlled, and in compliance, certain standard operating procedures (SOPs) must be adopted.
The importance of EM
Although both are essential and required by regulatory authorities, a robust environmental monitoring (EM) programme can be more important than sterility (or bioburden) testing to ensure the safe release of certain final products. EM is a key indicator that cleanrooms and all contamination control processes are working effectively. Through trend analysis, EM will enable risks from root causes (weather, season, poor cleaning, personnel changes, building system failure, etc.) to be proactively addressed before they become critical, resulting in costly product loss or, even worse, risk to the consumer.
By its very nature, sterility testing is not 100% effective: it’s destructive, so cannot test an entire batch. Furthermore, it can take up to 14 days to deliver a result. As some pharmaceutical products have a maximum shelf-life of 7 days and may even be used within 24 hours, the maths is clear; every precaution must be taken to ensure that product is manufactured sterile, with data trending and proactive maintenance of control through EM being key to minimising contamination risk.
There are a number of international regulations in place offering guidance regarding EM requirements. Core to all successful programmes, though, a company must create an SOP to dictate their own specific monitoring needs based on product type, sample frequency, locations and overall procedure.
The SOP should also standardise reactions to alerts or action level excursions and subsequent courses of action, such as secondary testing, immediate production shutdown or product quarantine. As laid out by the SOP, EM requires a strategic, scheduled sampling programme of predefined locations that generally dictates the type of sample taken and how.
Monitoring air
There are two common methods for airborne monitoring of viable micro-organisms.
Passive monitoring: Gamma-irradiated settle plates, usually 90mm Petri dishes, are widely used as they offer improved sterility assurance and extended shelf-life. Containing sterile growth media, these are exposed to the environment for a set time period prior to incubation to grow any viable micro-organisms that have settled on them during the exposure period (Figure 1).
Active sampling: This involves the drawing of a known volume of air over or through a sterile collection medium, allowing the user to readily quantify results. The number of samples and frequency would be determined by the grade of cleanroom and processes being done. Therefore, a risk assessment approach is the most appropriate.
The most widely used active sampling method involves direct, multipoint impaction on to a standard agar plate (Figure 2). Air samplers, such as the SAS range (Cherwell Laboratories, Bicester, UK) shown in Figure 3, use this technique and are available in different formats depending on monitoring requirements.
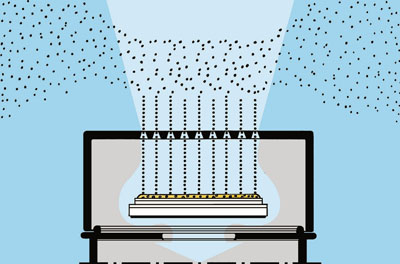
Figure 2: The direct, multipoint impaction method onto a standard agar plate used by SAS microbial air samplers

Figure 3: The SAS air sampler (Cherwell Laboratories, Bicester, UK) provides readily quantifiable microbial results as cfu/m3
The differing formats include flow rate, number of sampling heads (some units such as the SAS Duo 360 have two sampling heads), number of holes in the air sampler head, as well as isolator versions controlled outside the isolator. Crucially, air samplers should be regularly serviced and recalibrated (every 6–12 months) to ensure maximum confidence in monitoring data.
Monitoring surfaces and personnel
Surfaces, such as floors, walls and equipment, are regularly cleaned and monitored for viable counts using contact plates containing media that is general purpose for micro-organisms (Tryptone Soya Agar), or specific for moulds and yeasts (Sabouraud Dextrose Agar). As the media protrudes above the rim of a plate, it can be pressed against any flat surface to be sampled and then incubated. Any viable micro-organisms will grow on the surface to give a total viable count. Where the surface is not flat or is hard to reach, a sterile swab can be used to rub over the test surface and then subcultured onto a plate for incubation.
The greatest risk of contamination in a cleanroom arises from personnel. Therefore, the effectiveness of gowning must be regularly assessed and personnel alerted to flaws in their gowning technique. Contact plates are again used to monitor parts of the body, such as gloved hands or forearms. Petri dishes (90 or 140mm) are used as finger plates to monitor both the effectiveness of gloving and to monitor how the operator works. In an aseptic environment, it is vital that the operator does not touch any part of their bodies to avoid picking up micro-organisms. They must also regularly sanitize their hands and take care of what objects they touch.
Choosing your EM media
As mentioned previously, the two main media types used in environmental monitoring are Tryptone Soya Agar (TSA) and Sabouraud Dextrose Agar (SDA). The most important aspect of choosing an appropriate medium is ensuring that it can grow as wide a range of organisms as possible, especially the most common types associated with your own cleanroom. This should be ascertained when the EM regime is validated and by monitoring the isolates from your EM regime.
What you may not realise is that the disinfectants you use will probably leave a residue on the surface. This residue will not kill micro-organisms; but, in the case of surface monitoring, it may well prevent or inhibit growth on the agar surface. Therefore, most manufacturers of prepared media will offer TSA and SDA with suitable combinations of neutralising agents. If you have to comply with standards such as Good Manufacturing Practice (GMP), the regulatory texts, such as those of the European Pharmacopoeia, will list the inhibitory chemicals with suitable neutralisers.
If the disinfectant you use is not in that list, then your prepared media provider should be able to recommend the most appropriate neutralisers. In the case of swabs, a saline solution that contains the appropriate neutraliser can be used to wet the swab. It should be noted that your regulators may well ask for proof that the neutralisers that you are using are appropriate for the disinfectant(s) you use.
Regulatory changes
If your cleanroom manufacturing facility is operating to EU GMP, then a section from Volume 4 of the EU Guidelines to Good Manufacturing Practice — Medicinal Products for Human Veterinary Use, called Annex 1 – Manufacture of Sterile Medicinal Products, will be in use. Although your product may not need to be manufactured in sterile conditions, Annex 1 is the guideline used regarding cleanroom operation.
Annex 1 was published back in the 1990s and has been revised on numerous occasions since; the most recent was in 2009. It is now going through a major review for a number of reasons, mainly to keep up with advances in manufacturing technology, but also because of a loss of expertise as experienced practitioners retire. This has led to a requirement for this expertise to be written into the regulations.
To prepare people for the major revisions, members of the committee who are updating Annex 1 have been revealing areas that are probably being changed or amended for much of this year at peer group events and conferences. Amendments include a better clarification of environmental monitoring, such as how often monitoring should occur in lower grade areas and the definition of a “grade A air supply.”
There are also ambiguities in the current version that are going to be clarified, such as the meaning and interpretation of the term “average values” regarding microbial counts in the various cleanroom grades. Overall, there is going to be an increase in the number of pages from 16 to around 24. All company microbiologists will be studying the new version of Annex 1 carefully when it has been published, hopefully in early 2017.
In conclusion: proactive EM is key
To ensure the ongoing effectiveness of control measures and to assess the contamination risk of final product, a well-planned and implemented EM programme is essential. By producing trending data, an EM programme ultimately enables the proactive, rather than reactive, management of contamination issues before they become critical and prevent product being shipped, or even recalled, which ultimately saves money and crucially ensures safer products.




